Brooke Shields broke her femur in January when she fell off a balancing board at her gym. At the time we were at the height of the pandemic and Brooke had to spend a lot of time alone at the hospital relearning how to walk. Then Brooke got a staph infection, complicating her recovery. During a recent event for Marie Claire, Brooke said that she chose not to take painkillers stronger than Tylenol. Brooke did not want to become reliant on opioids. She also wanted to understand and recognize her pain so that she could monitor her injury. Below are a few more highlights from People:
Shields, 55, never took anything stronger than over-the-counter drugs like Tylenol out of concern that she would form a reliance on opioids like OxyContin or Vicodin, she tells PEOPLE.
“I didn’t want to leave the hospital with no pain, get home, and think I was dying, because the pain was excruciating,” she explains after speaking at The Marie Claire Power Trip: Off the Grid event. “I was like, ‘I’d rather have excruciating pain in the hospital.’ ”
Shields also wanted to make sure that over the course of her recovery, she was able to recognize the difference between the pain from her original injury and anything new that could crop up.
“[I wanted to] get used to it and understand what’s pain and what’s further injury, because what happens is when you start to feel pain, you think you’re injured again, but you might not be as injured. You just might be sore or in pain,” she says.
“I wanted to really understand what kind of pain it was, because when you leave, and you go home, and you feel pain, you get really scared,” she adds. “And I wanted to at least go, ‘Oh, I felt that pain before. Okay.’ You don’t feel sort of like a victim to it.”
The mom of two, though, found that it was hard to convince the hospital staff — “I said, ‘What’s the over the counter thing that I can take at the highest dose where it’s safe? And I won’t leave with a prescription.’ And everybody wants to give you Oxy.”
Shields feels as though the reliance on intensive painkillers is “part of the whole epidemic” with opioids that is hurting people all around the country.
She adds, though, that her decision not to take opioids “is not about being a hero.”
When I first saw this headline, I thought it was a humble brag. When I read why Brooke skipped opioids despite being in excruciating pain, it sounded like a very smart move. Since Brooke was relearning how to walk, being able to recognize different pain may have helped her avoid further injury. I believe Brooke when she said that everyone were pushing Oxy on her. I have a high pain threshold, however I know broken bone pain and am not sure how Brooke tolerated that. She must have tapped into a deep reservoir of determination. Being able to state your boundaries with doctors is no easy feat either.
I am so happy that Brooke is still with us. Dealing with a broken and infected femur at a time when you cannot see family must have been difficult for Brooke. Brooke found her strength and was able to make it out on the other side to tell the tale. Hopefully, Brooke’s story will help other women advocate for themselves within the medical system. I also hope these pharmaceutical companies will find a less addictive drug to help people manage pain.
Photos credit: Instar and via Instagram











After having 2 knee replacements within 6 weeks of each other I have learned many things. One was that you want to manage the pain. I understanding not wanting to take an opiod pain killer but to be in excruciating pain can impede your progress. I was given 2 different pain killers and chose the one that less potent. Both times I had the pain under control within a week and could switch over to strictly Tylenol. I have a high pain tolerance and really don’t like taking prescription pain killers because they weird me out. But I took my doctor’s advice to control the pain (and if that was with just Tylenol he was good with it). It can be done using prescription meds and you can understand it without being in excruciating pain.
I can absolutely relate to what she is saying.
When I gave birth, I really wanted to feel everything. It felt comforting to feel the contractions increase in strength. And I really felt the baby being pushed down by my body on my second birthing experience. It’s great to have this opportunity but it’s not always possible.
Pain can be extremely debilitating and it can kills us!
I get what she’s saying but may I just say as a chronic pain patient; this is still a humblebrag. We don’t actually NEED to know about people’s pain killer usage (notably, few people are like “I broke my femur, took my medication responsibly, and still relearned to walk with the assistance of medical professionals” because that doesn’t make an interesting story).
Pain killers are medicine. Yes, medicine that needs to be monitored and used responsibly, but medicine.
As another chronic pain patient, she is welcome to know my daily bladder screaming and burning. A UTI that never heals. I “know” more than I care. I’m happy for her pain free life.
@Sarphati I’m so sorry. It sounds a lot like Interstitial Cystitis, which I also have. Life would be unbearable without Amitriptyline.
My Mom actually had something similar for several years, eventually, they found diverticulitis (I belive it was) of the urethra. They were able to do surgery and remove it but it was VERY difficult to diagnose and she was in pain every single day.
I’m so sorry.
Is the description of opioids as painkiller normal in the US?
I never heard of opioid for broken bones bevor, only for really bad pain (cancer, burns, some cases of chronic pain, ect.) and very strictly controlled.
I was told, pain is usually an indicator how much you can do again and should not be removed completly, only managed, to ensure you don´t overdo it. At least in cases, where a complete recovery can be expected.
Unfortunately yes. I’ve been prescribed opioids following a root canal, after foot surgery, after having a very easy birth, and after slicing my finger open. And each time, the prescription was for like two weeks of pills. The only time I ever needed them was after my foot surgery and even that was only for a couple days immediately after. Opioids are incredibly over prescribed both in instances and quantity.
Omg. No wonder there are so many people with opioid addiction. I always wondered how that happened.
Here you need a special prescription from a specialist for pain management to get opioids outside the hospital at all. And you have to hand it in at a pharmacy licenced for opioids.
(My grandfather got morphium for terminal cancer, you have to document every drop and return it if anything is left.)
I had a doctor insist on prescribing it after a very minor procedure, which I had already had done once and didn’t need anything more than a single tylenol. I said no thanks, and they wrote it anyway. This was many years ago, but it’s bothered me ever since then.
I did have to take it after absolutely destroying my ankle and needing surgery, but I stepped down each day and was off it within a week. I was lucky to be able to do that, many people can’t.
I’ve got three bottles of percocet (I am aware that it is not as addictive as oxy) just laying around- never took them, but the ones I received were for 5-7 days rather than 2 weeks. I had 3 poorly healed metatarsal fractures that I had revised in march, and I took one the first night. I do *not* like how they make me feel in my head, so I took max ibuprofen every 8hours, overlapping midway with 1gm tylenol every 8hours. Did a pretty damn good job. I also feel like if pain is completely removed, you risk worsening the condition. If I were a chronic pain patient, on the other hand, I don’t know that I would feel the same way. I think I’d be looking at a variety of modalities to treat it.
I was sent home with a 2-week supply of Vicodin after my partial hysterectomy (full abdominal incision). I only took a few before stopping because they made me very constipated, and the straining to go was painful and putting too much stress on my incision. After quitting, I realized I wasn’t really hurting that much and could manage just fine with a little bit of ibuprofen. When I broke my ankle a few years later, the hospital sent me home with a prescription for opioid painkillers, but I didn’t fill it because I just wanted to get home after spending 5+ hours in the ER. Again, I was okay without it, so i guess I have a pretty high pain threshold. I consider myself fortunate, not virtuous; I really feel for those who are suffering and have to risk addiction because opioids are their only relief.
This is of course my own experience , but I have a chronic back and neck injury and this is exactly what I did to learn how to move, when to rest, what kind of movements to avoid. Pain is a signal and when you don’t feel it you do things that aren’t always the right thing to do and you continue longer than is healthy.
Exactly right.
I agree with her comment about being offered opioids; most recently happened when I had surgery a few years ago. I was fortunate to only have minimal pain and took Tylenol in the hospital, yet was offered a month prescription for Oxy with the option to get 3 refills.
I also wonder, as Brooke’s mother had addiction issues and she has been around long enough to see her industry peers (Michael Jackson for starters) issues with prescription meds, if that was part of her decision.
I cannot believe that the Dr who prescribed so illegally isn’t getting slapped around by the DEA. MDs have to have a unique DEA number to prescribe and their prescription writing is monitored to prevent exactly this. You should make a complaint to your state’s board of medical licensing and ethics.
Not mentioned, Brooke spending her entire young life dealing with her mother’s alcoholism. Knowing that is in your genetic heritage can turn what should be pain relief into a long series of PTSDish worries and flashbacks.
Also, the asshole hospital gave her the staph infection. The rates for those vary widely, based on how closely the hospitals follow anti infection protocols. So I would have a huge reason to not listen to them. I don’t know if she went back to the same hospital or not.
Infection control is probably the most challenging aspect of hospital management, because it relies on EVERYBODY doing their part. All it takes is one individual deviating from procedure to have things go awry. Anybody being admitted to the hospital (or family/friends acting as the patient’s advocate) has my blessing to be an a-hole and call out personnel who appear to be acting carelessly. It’s perfectly okay and within your rights to ask someone taking blood, doing a procedure, etc. something like, “Did you wash your hands just now? No? Then please don’t touch me until you do.”
COVID complicates the situation because hospital visitors have been severely restricted or outright banned. Friends and family can’t advocate for patients who are too ill to advocate for themselves. It’s a shame that patients/friends/family have to do that legwork, but employees doing direct patient care are stretched pretty thin, and unfortunately some succumb to the pressure to save minutes and/or supplies by cutting corners.
In the immediate aftermath of a break or surgery, it’s not particularly important to heed your pain to know what you can do. It’s way more important to get good rest, which severe pain inhibits. I’ve taken Vicodin several times for short periods to get over that first trauma response and it was great for that. (Of course, I am not an addict and would make a different choice altogether if I was/had those tendencies!) I agree with her that once you’re actively trying to heal (vs. recovering from immediate trauma) pain is helpful.
That said, everyone’s pain tolerance is different. Where I needed Vicodin, someone else might be fine with Tylenol, while another person might need something stronger. Overworked nurses and doctors can’t always tell who’s who, so it’s important to advocate for yourself.
And chronic pain is a whole different animal. I wish those of you with chronic pain the best pain management science has to offer you!
I had 2 surgeries in different countries (one in the states, the other in kh home country). For the one in the states which was an appendectomy, I was prescribed oxycodone and after my prescription ran out, my doctor kept pushing it on me (I declined several times since I hated it). The second surgery which was a deviated septum one, I was prescribed an over the counter anti inflammatory pain killer. So yes absolutely the US overprescribes pain killers and opioids, it’s really concerning
This is totally off topic, but I love those brown boots Brooke is wearing in that last photo. I want those boots!
Those are the same boots Katie Cambridge wears!
My nose surgeon said that if ibuprofen or acetaminophen were developed today, they would be controlled by prescription rather than over the counter. They work really well when monitored. But people do need stronger stuff sometimes. I don’t think she was saying that she was doing it without managing the pain, just without the stronger stuff that she would be wary of as a child of an alcoholic.
Probably, especially the acetaminophen, that can be very dangerous on its own.
Only if you have liver disease or exceed the max recommended dosage. It will cause liver failure if overdosed.
Ibuprofen used to be prescription only. I used it for menstrual cramps in the ‘80’s and needed a scrip.
I’ve given birth three times, fell down the stairs holding a baby and 6 months pregnant, and broke my foot in my 30s. I’m not able to speak to chronic pain, but my personal experience is that ibuprofen helps way better than any narcotic. Opiates make me feel sick and anxious, and honestly I’m grateful for that reaction.
I completely respect Brooke made the best choices for her and she was free to do so for her own body and the process and experience she wanted. No problem with that. BUT I wish we would not be talking of refusing painkillers because they might lead to an opioid addiction: painkillers have a legitimate role to play and it should be an individual’s own choice.
Personal note (this is why I am upset [not at Brooke!]): I was going to get eye surgery and the doctor said she would not prescribe me painkillers because she didn’t think the pain would be that bad and she was worried it would cause an addiction. (Recovery time was two weeks and the proposed surgery involved cutting off and reattaching an eye muscle. I have esotropia.) Okay really? Now who would know better what the pain felt like and how bad it would be than I would, having to experience it in my own body? I decided not to work with that doctor. Note, I have no history of addiction. If people want to use painkillers responsibly when needed, I don’t see that as a problem. I’m not going to suffer pain just because some other person thinks “oh it’s not that bad” — when I’m the one who’d actually be suffering it.
@Emma I’ve had eye surgery and was not given enough of a relaxer for the time I was in surgery and I will never make that mistake again (I had to be awake during the procedure). I understand your pre-surgery concerns. I was only given over the counter meds for recovery – not strong enough. So, for what its worth, I think you made the right call!
I agree with this so much. I’ve had surgeries and sports injuries where stronger pain control allowed me to rest the first few days on my way to recovery. I don’t find doctors pushing them on me, but seem to be responsible and helpful with detailing how to mix in Advil, etc.
I’ve been watching DopeSick and that makes me never want to try Oxy ever so I don’t blame her, that shit can ruin your life.
Agree. Although I will say Dopesick is an amazing show. Production value makes each episode feel like a movie. Top-notch acting as well.
As others have said above, alcoholism runs in her family, and she is smart to respect that. I can imagine the pain was excruciating – I have read that the femur is the biggest bone in the body and just horribly painful when broken. I admire her bravery here, what she went through is no joke. And good for her for advocating for herself!
As a chronic pain sufferer, I side-eyed her comments at first but then I remembered how her mother’s alcoholism shaped Brooke’s life. That profoundly affected Brooke and I can respect that she has a healthy fear of developing an addiction because of it. That being said, my mom recently broke her elbow and said it’s worse than childbirth, even with painkillers, so I have no idea how Brooke managed to cope with a femur break.
Watching ‘Dopesick’ on Hulu and have to say that after seeing that I think I’d opt for Tylenol only to deal with pain. Completely understand that everyone has different pain tolerance and that has to be part of the equation but the idea that you should feel NO PAIN or minimal pain during recovery isn’t realistic. Perdue Pharma made us believe ‘pain is bad and must be treated’ when it’s not bad, it’s a signal from the body. I give Brooke a lot of credit – with her genes, she clearly didn’t want to risk things getting out of hand is opioids.
A few years ago, I had my gallbladder removed. When I came out of the anesthesia,
I quickly realized my entire body was on fire and itching like crazy. Turns out the surgeon had ordered oxy be given to me intravenously to control any pain upon my awakening. The allergic reaction was by far the most severe complication of the entire surgery and as a result, I wound up having to spend an additional two days in the hospital.
I was furious no one consulted me about oxy prior to surgery – I’d most definitely have refused any pain meds outside of Tylenol, Advil or Aleve because addiction runs rampant throughout my family going back at least three generations. I certainly don’t judge people who need it (it was the only thing that spared my dad from unbearable pain when he was dying of cancer), but I *do* judge doctors who administer it without consent.
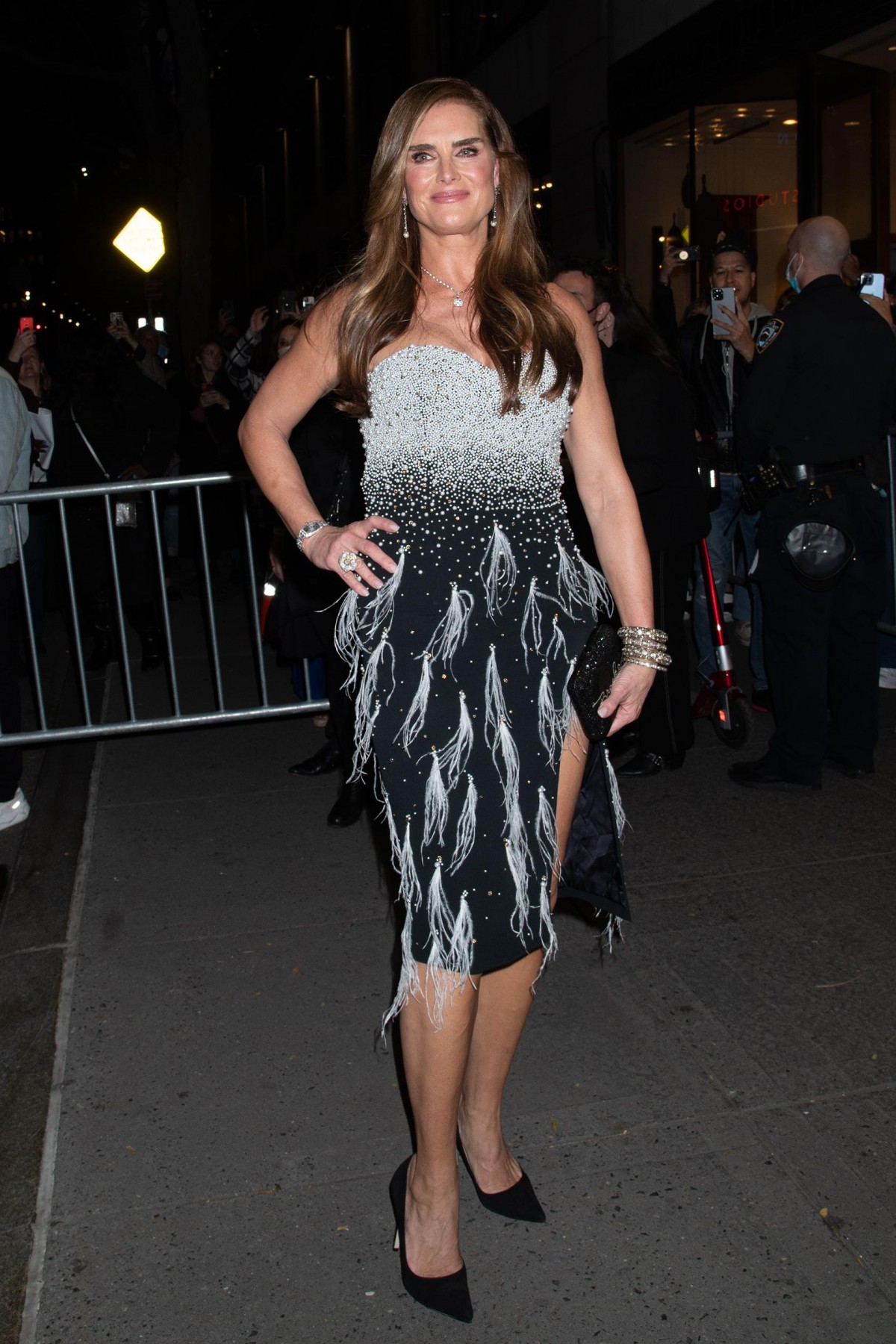
P.S. are those recent pics of Brooke? She looks AMAZING.
I had a staph infection and was prescribed OxyContin. Staph or MRSA in my case, literally feels like your flesh is being liquified from the inside. However, I can see why she didn’t take Oxy the whole time because MRSA is really hard to eliminate. It takes multiple courses or antibiotics, so feeling the pain is an indicator that you should get some more antibiotics or treatment before it eats more of your flesh.
I had a very bad trimalleolar fracture. After they set it there was so much swelling they had to wait almost 2 weeks before they did surgery to repair it. So for two weeks everytime i shifted in bed or managed to get to my bedside commode the bones would grind together. I was in a open partial cast.
I have a very high pain tolerance but no one is that high, she’d be taking painkillers for the break i had.